30/5/19
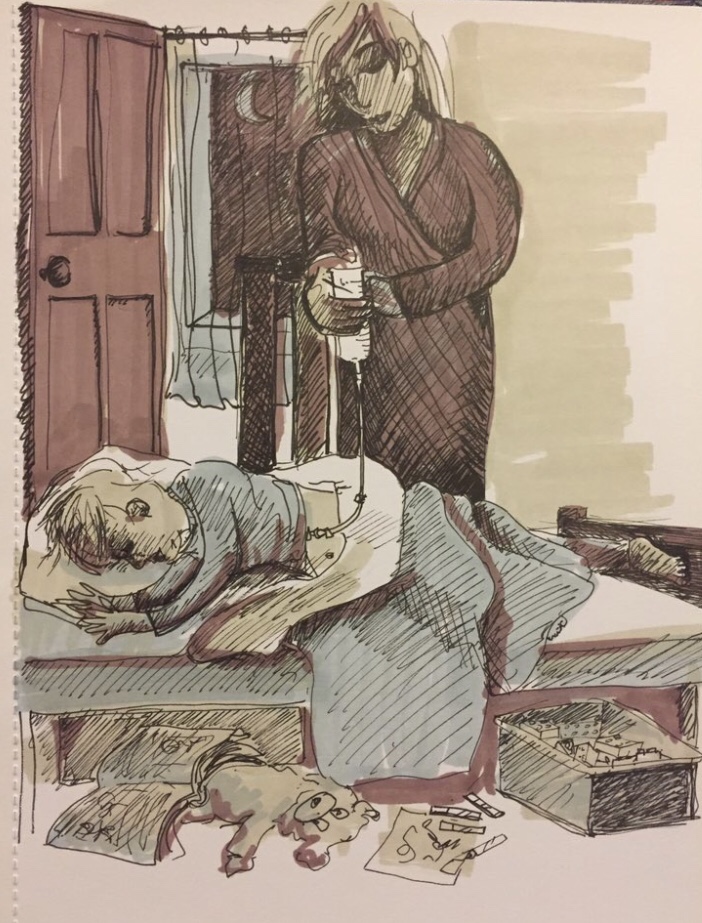
You may know that I’m a Children’s Nurse who initially trained as a Registered General Nurse back in the late 1980’s. My experience of caring for people with mental needs includes caring for a skeletally year thin young lady with anorexia nervosa on a general medical ward who required intravenous fluids. I struggled to understand why she couldn’t and wouldn’t eat and if I’m honest was totally overwhelmed as an 18 year old seeing her emaciation that wasn’t attributed to a physical health issue. Later in my training I spent a summer on a placement at Whitchurch Hospital in Cardiff, my memories of that time include enjoying the beautiful grounds with the patients being cared for, as well as accompanying patients to and from their ECT treatments. Much of my time was spent ‘being with’ people, not always chatting, just ‘being’. I remember a ward sister (who I respected greatly) remarking that that she didn’t think I’d make a mental health nurse, it takes all types to make the world turn I tell myself, as a result I have huge respect for my mental health nursing colleagues for the work they do.
As I moved throughout my career I’ve focused on nursing children and young people with renal, oncology and general paediatric ‘physical’ health related needs. Emotional well-being was an underlying theme throughout my career and whilst the mental health needs of young people have much greater focus than they’ve ever had previously, it’s something I’m still trying and if I’m honest often struggling to understand.
The Mental Health Foundation flags that while most children grow up mentally healthy, data suggests that more children and young people are having challenges with their mental health today than 30 years ago, they suggest its probably because of changes in society and it’s impact on feelings and behaviours. The transition to adulthood may also include experimenting with alcohol, drugs or other substances that can affect mental health too.
1 in 10 children and young people experience mental health issues and these can be a direct response to what is happening in their lives, issues such as:
- having a long-term physical illness
- having a parent who has had mental health problems, problems with alcohol or has been in trouble with the law
- experiencing the death of someone close to them
- having parents who have separated or divorced
- being separated from the family resulting in them becoming ‘looked after’ by their local authority
- having been severely bullied or physically or sexually abused
- living in poverty or being homeless
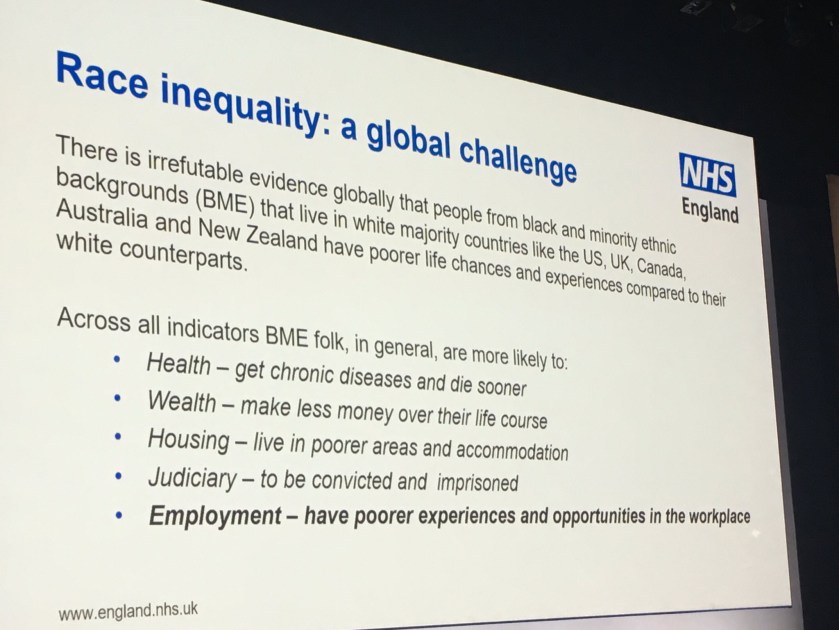
- experiencing discrimination, perhaps because of their race, sexuality or religion
- acting as a young carer for a relative, taking on adult responsibilities
- having long-standing educational difficulties.
I’m sure there are no doubt things that have been missed from this list. We’re all far more aware of ACEs ‘Adverse Childhood Experiences’ http://www.healthscotland.scot/population-groups/children/adverse-childhood-experiences-aces/overview-of-aces than ever before and the impact they can and do have on mental health and well-being.
Children and Young People don’t always know or are able to articulate what these adverse experiences are, leading to the complexity of management and care. On chatting to my 15 year old daughter, she offered the wisdom only a 15 can ‘see mum it’s not just about one thing, it’s often multiple stuff, the constant layering of difficult hard life things that makes life tough sometimes’. Beautifully put I think!
This infographic from Healthy London Partnership provides an overview of the challenges children and young people face in London.

The types of mental health issues children and young people can present with include:
- Depression, this affects more children and young people today than in the last few decades, but it is still more common in adults. Teenagers are more likely to experience depression than young children.
- Self Harm is a very common problem among young people. Some people find it helps them manage intense emotional pain if they harm themselves, through cutting or burning, for example. They may not wish to take their own life.
- Generalised anxiety disorder (GAD) can cause young people to become extremely worried. Very young children or children starting or moving school may have separation anxiety.
- PTSD or Post traumatic stress disorder can follow physical or sexual abuse, witnessing something extremely frightening of traumatising, being the victim of violence or severe bullying or surviving a disaster.
- Children who are consistently overactive (‘hyperactive’), behave impulsively and have difficulty paying attention may have ADHD Attention Deficit Hyperactivity Disorder.
- Eating Disorders usually start in the teenage years and are more common in girls than boys. The number of young people who develop an eating disorder is small, but eating disorders such as anorexia nervosa and bulimia nervosa can have serious consequences for physical health and development.
Shockingly the leading cause of death in the 5-19 age group is death by suicide according to the Office for National Statistics http://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregisteredinenglandandwalesseriesdr/2015#number-of-land-transport-accidents-among-5-to-19-year-olds-decreases-in-2015
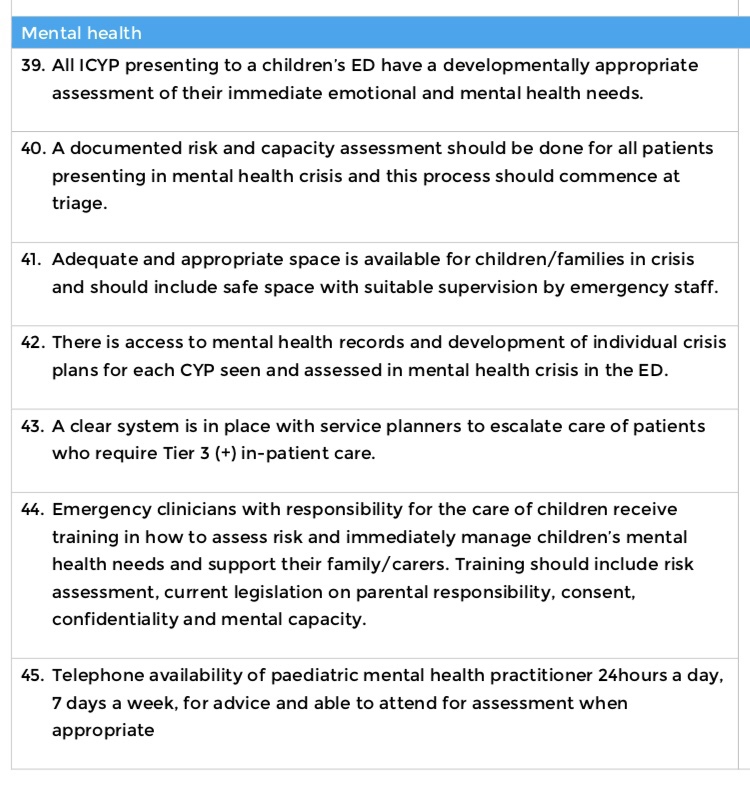
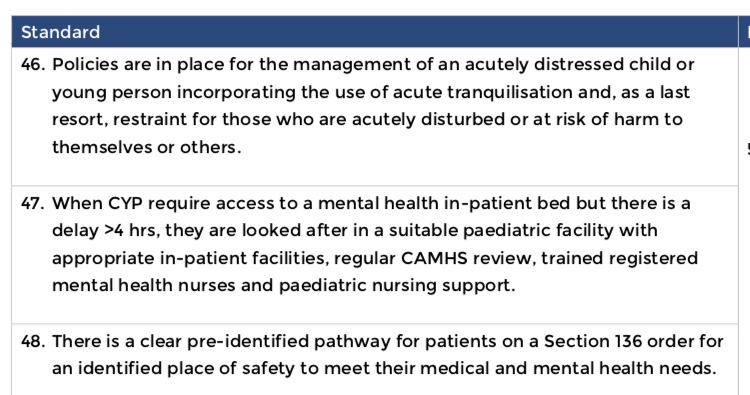
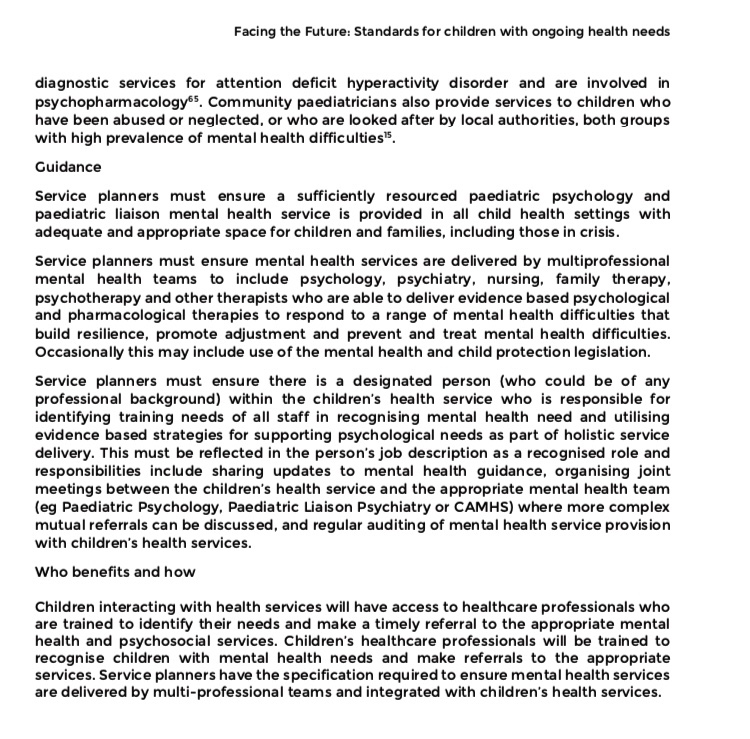
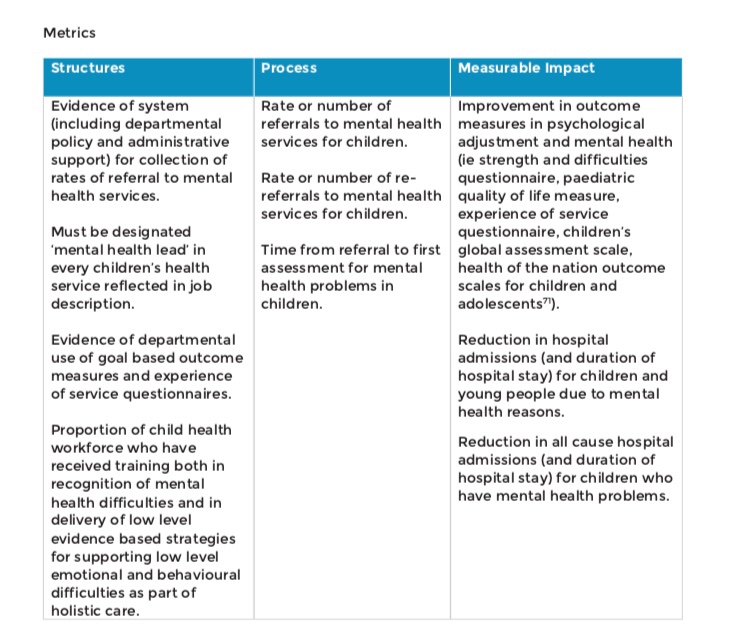
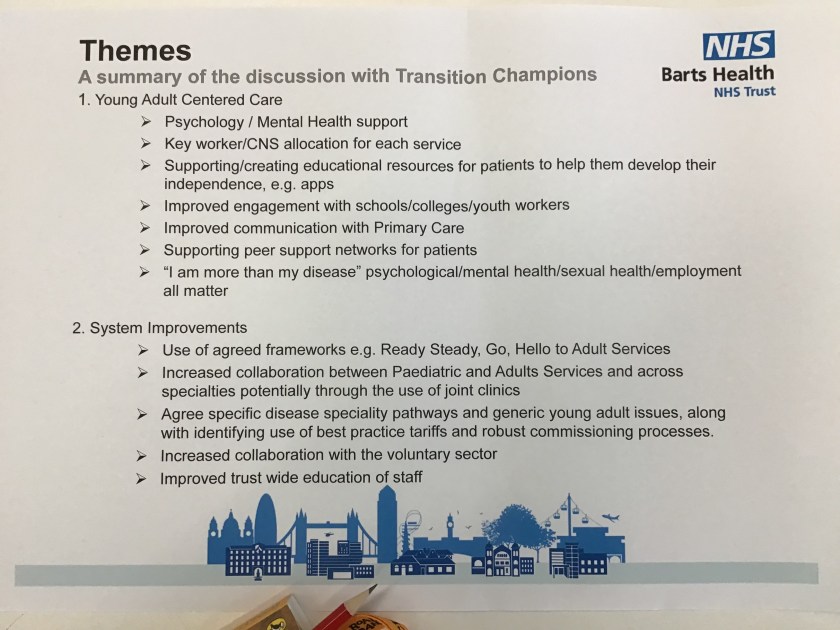
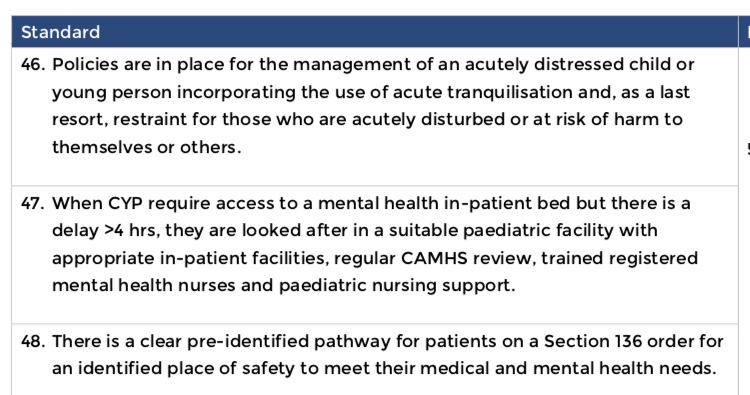
Some of the children with mental health needs as we know present in Emergency Departments. The RCPCH in their ‘Facing the future’ Emergency Care Standards https://www.rcpch.ac.uk/sites/default/files/2018-06/FTFEC%20Digital%20updated%20final.pdf sets out what we need to be able to offer. 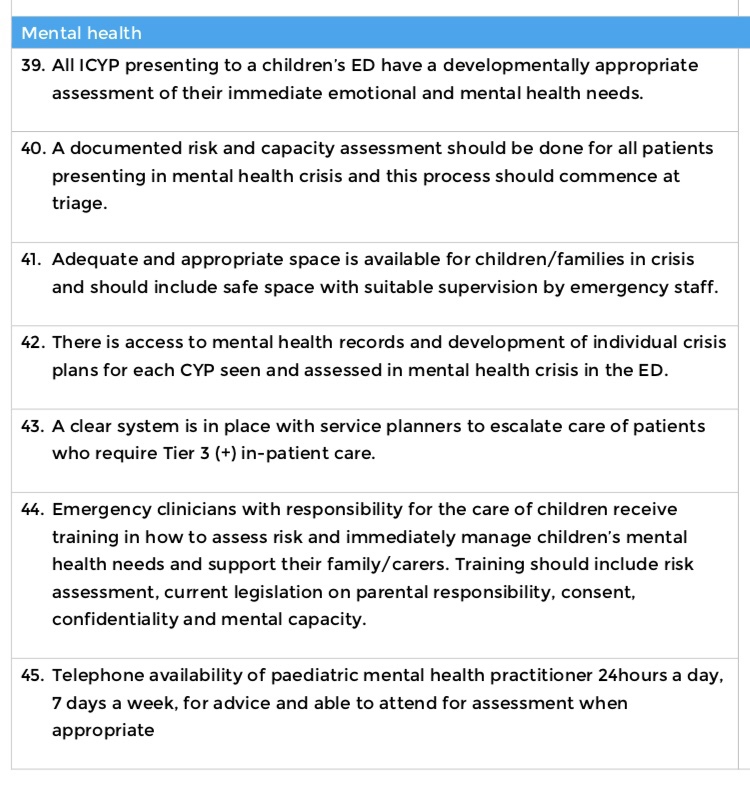
The emerging crisis intervention and home treatment models of caring are hugely helpful in supporting children and young people in areas other than ED, it’s a far from therapeutic environment for those in mental health distress.
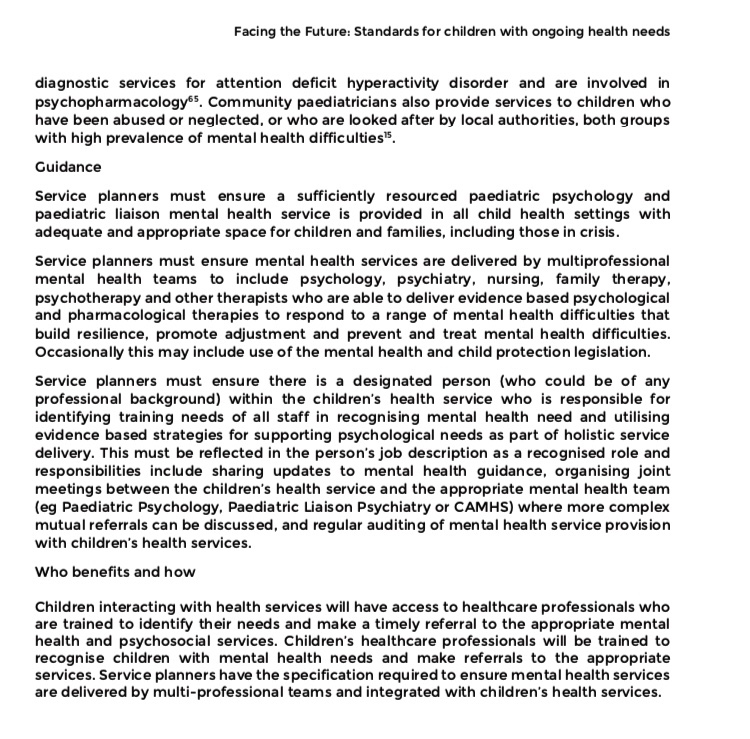
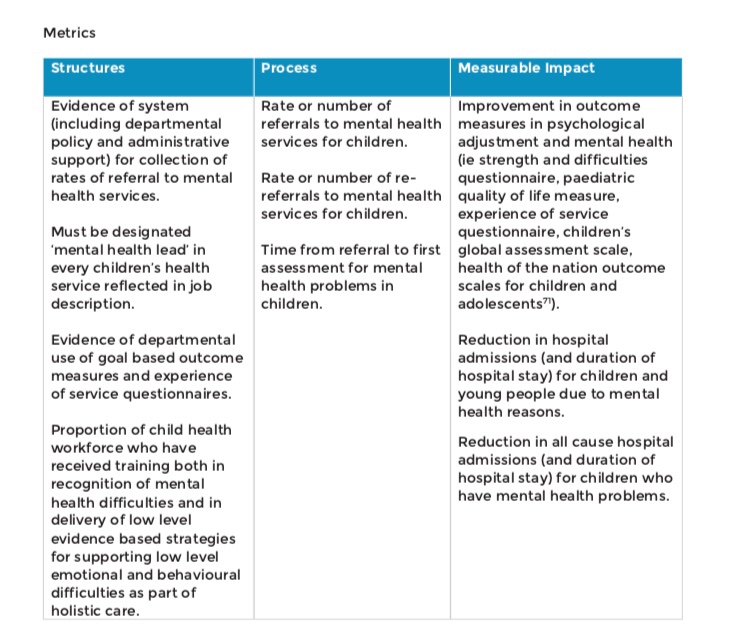
Of course we also need to support and provide support for the mental health of children and young people with complex ongoing health needs too, the RCPCH Facing the Future sets out the standards required https://www.rcpch.ac.uk/sites/default/files/2018-04/facing_the_future_standards_for_children_with_ongoing_health_needs_2018-03.pdf


We also need a workforce that has the skills to engage with children and young people, the @WeCanTalk programme developed by @RobinfromCAMHS in collaboration with young people and staff is a great example of addressing support and education of staff. Our skills as professionals to connect with children and young people to build trust, foster understanding, show value, respect and creation of safe spaces are key.
Our local mental health services NELFT and ELFT have been so welcoming to visits and collaborations, partnership working across STP patches has to be a key element of future working. Thank you @Nicola21762634 for hosting me this week, I learnt so much! Hoping to meet @bewseyr soon too.
Just as we’ve reflected on the opportunity to consider a RN Child/LD pathway to qualification in recent weeks, I wonder if going forward we could offer a RN Child/MH pathway? Perhaps it already exists? It surprises me that we have adult MH trained nurses caring for CYP and I think we encourage more Children’s trained nurses to work in MH settings?
And of course there are clear opportunities to ‘prevent’ and reduce deterioration of mental health illness too. As people who are passionate about children and young people’s well-being we can all promote and role model the importance of
- being in good physical health, eating a balanced diet and getting regular exercise
- having time to play, indoors and outdoors
- support being part of a family that gets along well (most!) of the time
- encourage taking part in local activities such as attending voluntary organisations as well as opening up volunteering opportunities.
- support going to a school that looks after the physical and emotional wellbeing of all its pupils, do we have governors who lead on well-being in all our schools?
I wonder what more we can do to work in partnership with schools too? The Schools Mental Health toolkit developed by the Healthy London Partnership team can be used to promote wellbeing in schools https://www.healthylondon.org/resource/schools-mental-health-toolkit/
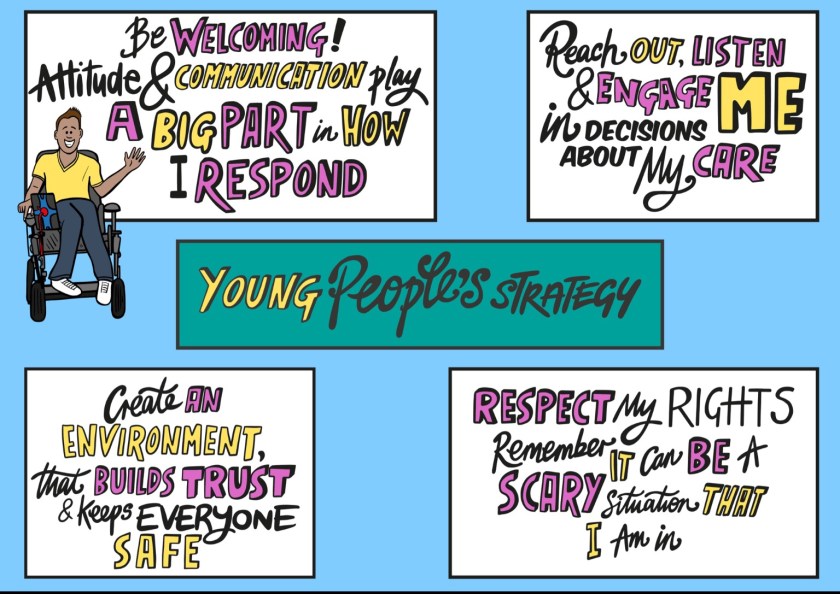
These are the ‘asks’ from young people to schools which are powerful calls to action:

I also think we can do more investing and valuing of school nursing https://www.rcn.org.uk/-/media/royal-college-of-nursing/documents/forums/children-and-young-people/staying-healthy-forum/school-nurses-toolkit-2017.pdf, ensuring they have the skills and insight to support the mental health needs of pupil and the staff that support them. Why not recruit mental health nurses to be school nurses?
And what opportunities does Social prescribing offer Paul Jarvis-Beesley, Head of Health at StreetGames @PaulWJarvis blogs about what this can offer here https://www.ukyouth.org/2019/03/05/social-prescribing/
This is clearly a conversation that will continue, please do follow…
@CYPMentalHealth http://cypmhc.org.uk/
@YoungMindsUK https://youngminds.org.uk/
There are loads of really helpful resources from the @rcpsych that are worth dipping into too, they’ve got a great short film on anxiety https://www.rcpsych.ac.uk/mental-health/parents-and-young-people
@EmmySelby is a mental health nurse who is really keen to support digital development and be creative, do follow her on twitter.
@lizziebessell is an ED Matron who’s been awarded a Florence Nightingale Fellowship to explore how we can best support young people with mental health needs in acute hospital settings.
I’d really value hearing more about the challenges faced and the solutions that you’ve put in place to address some of the challenges…..
Have you employed Mental Health Nurses in general paediatric areas, what difference has this made?
Have collaborations with Mental Health Teams brought benefits? Are you working with primary care on this agenda?
Love these prompts from young people to parents 


 As the political landscape is so chaotic a number of Children’s Charities have grasped the opportunity to seek help from the public to ask the new Prime Minister to set out their ambition and commitment to children, will you ask them to too? here’s the link to speak up for children… https://act.childrenssociety.org.uk/page/43598/action/1?locale=en-GB
As the political landscape is so chaotic a number of Children’s Charities have grasped the opportunity to seek help from the public to ask the new Prime Minister to set out their ambition and commitment to children, will you ask them to too? here’s the link to speak up for children… https://act.childrenssociety.org.uk/page/43598/action/1?locale=en-GB